Learn about the different types of lipedema, the causes, the symptoms, the different stages as well as various treatment options including compression garments!
WHAT IS LIPEDEMA?
Lipedema is a chronic fat distribution disorder that typically manifests on the legs, buttocks, and in some cases arms. Lipedema affects both sides of the body equally and occurs almost exclusively in women.
Lipedema, especially in the early stages, can be misinterpreted as lymphedema or obesity. Lipedema is indicated by the build-up of painful fatty tissue, which is not present in overweight people. Therefore, lipedema is also called lipohyperplasia dolorosa: increased, painful fatty tissue.
CAUSES OF LIPEDEMA
The causes of lipoedema are still not yet fully known. However, as the condition occurs almost exclusively in women, and symptoms usually present or worsen at the time of puberty, pregnancy, or menopause, there is likely a connection to hormones. In addition, genetic predisposition can play a role in the tendency to develop lipoedema.
WHAT ARE THE SYMPTOMS OF LIPEDEMA?
The typical symptoms of lipedema are a large lower half and column-like legs, which are often tender and can bruise easily. It is typical to experience a larger difference in size between the upper and lower halves of the body. Unlike Lymphedema, Lipedema affects both sides of the body equally.
Lipedema occurs almost exclusively in women. The onset of lipoedema symptoms is often associated with weight gain that is connected to hormonal changes - such as puberty, pregnancy, use of birth control pills, and menopause.

Other possible signs of lipedema include:
- Fat build-up in buttocks, thighs, calves, and in some cases the arms.
- Exercise, elevating your legs, and support stockings do not help to reduce the fat/edema in the affected areas.
- There is typically no swelling in feet or hands.
- Pain, discomfort, or heaviness in the affected areas
- Affected areas can bruise easily
- Skin can appear dimpled like orange-peel
- Difficulty walking/reduced mobility
- Skin can appear dimpled like orange-peel
STAGES OF LIPEDEMA
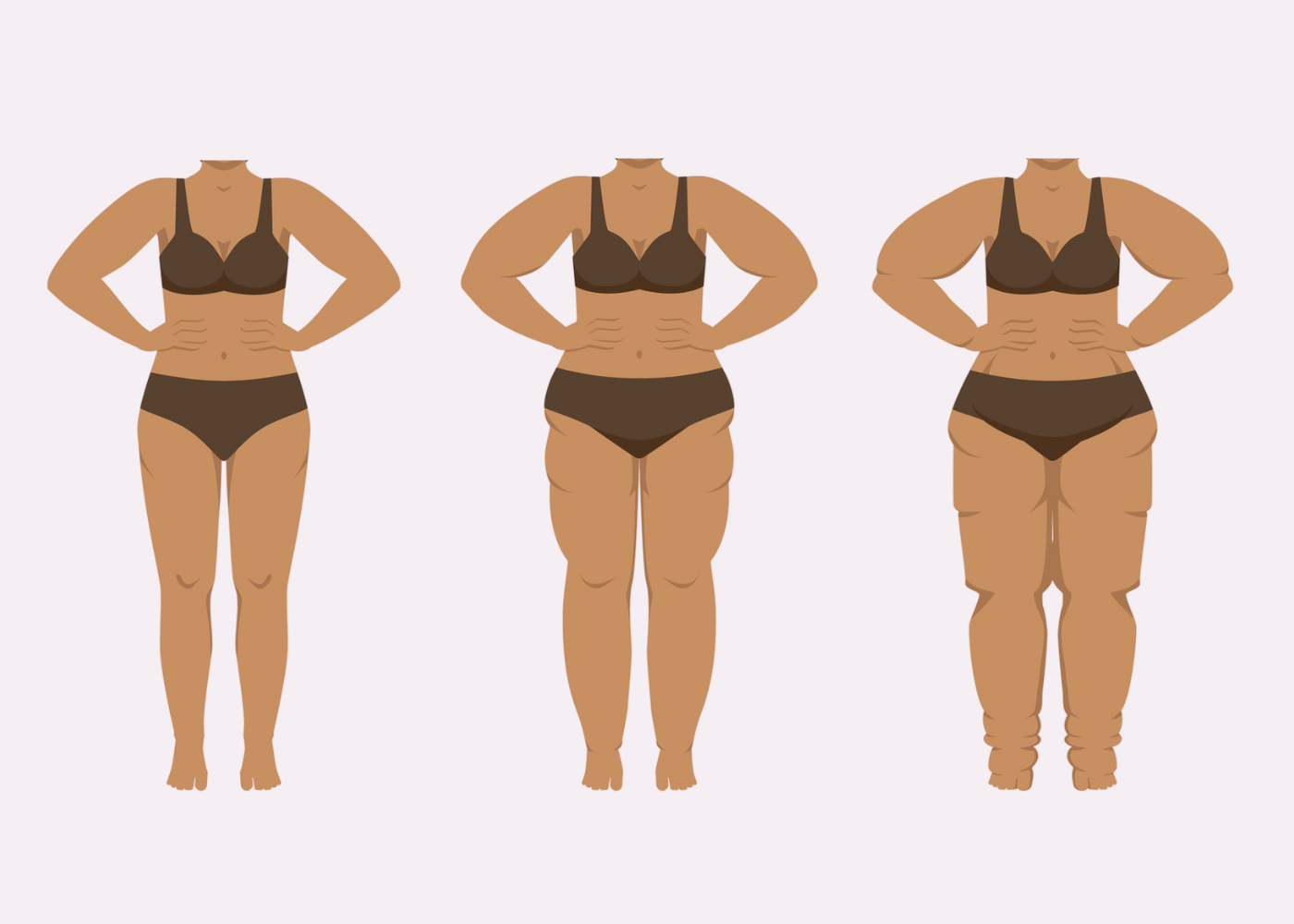
Stage 1: The surface of the skin is smooth, the subcutaneous adipose tissue is thickened, and the fat structure is finely knotted.
Stage 2: The surface of the skin is uneven and the fatty structure features coarse nodules.
Stage 3: In addition to Stage 2 symptoms, the tissue is coarser and harder as well. There are also lobes of fat causing extensive deformation.
TREATMENT OF LIPEDEMA
Lipedema is a chronic, sometimes progressive disease and therefore currently incurable. The goal of lipedema treatment is to relieve swelling and pain and thus improve the quality of life of the patient. Treatment for lipedema falls into two categories, conservative and invasive.
Conservative treatment for lipedema typically includes elements of Complex Physical Decongestion Therapy (CPT). CPT consists of manual lymphatic drainage, compression therapy, exercise therapy, skin care and self-management. The use of Intermittent Pneumatic Compression (IPC) can also be a successful form of treatment to help reduce limb swelling.
Invasive treatment for lipedema includes surgical interventions and procedures such as liposuction or a lipectomy. Following invasive treatments such as these patients will typically benefit from the more conservative treatment options such as compression therapy, exercise and MLD in order to continue to manage their condition.
We will discuss the five pillars of CPT in more detail below.
OBESITY AND LIPEDEMA: UNDERSTANDING THE DIFFERENCE

Lipedema and obesity are two completely different conditions with different causes, symptoms and treatments. Obesity is defined by the World Health Organization as "abnormal or excessive fat accumulation that presents a risk to health". The causes of obesity can vary but at its core the fat is a product of a prolonged calorie surplus. Obesity affects both men and women and the fat is typically distributed throughout the entire body.
Lipedema, on the other hand, is a chronic fat distribution disorder that primarily affects women. While the exact cause is still unknown, it is often triggered by hormonal changes that occur during puberty or pregnancy, for example. This leads to increased subcutaneous fat, which primarily affects the lower half of the body. In addition, the fat caused by lipedema is resistant to diet changes and exercise while in obese patients these factors would have an effect.
Unfortunately, both conditions often overlap: it is possible that accompanying obesity can worsens the symptoms of lipedema. The additional fatty tissue can increases the strain on the body, and the insulin resistance associated with weight gain increases the risk of developing secondary lymphedema.
LIPOLYMPHEDEMA: SECONDARY DISEASE OF LIPEDEMA
If left untreated, lipedema can continue to develop. Accompanying obesity in particular causes the leg circumference to steadily increase and eventually leads to water retention. While the lymphatic system can still function completely normally in the first few years, the increasing pressure in the leg has a disruptive effect on the lymphatic vessels. This increasingly impairs the lymph flow. Therefore, many patients who suffer from untreated lipedema sooner or later develop a lymphatic drainage disorder, i.e. lymphedema. In this case, it is referred to as "lipolymphedema" or stage IV of lipedema.
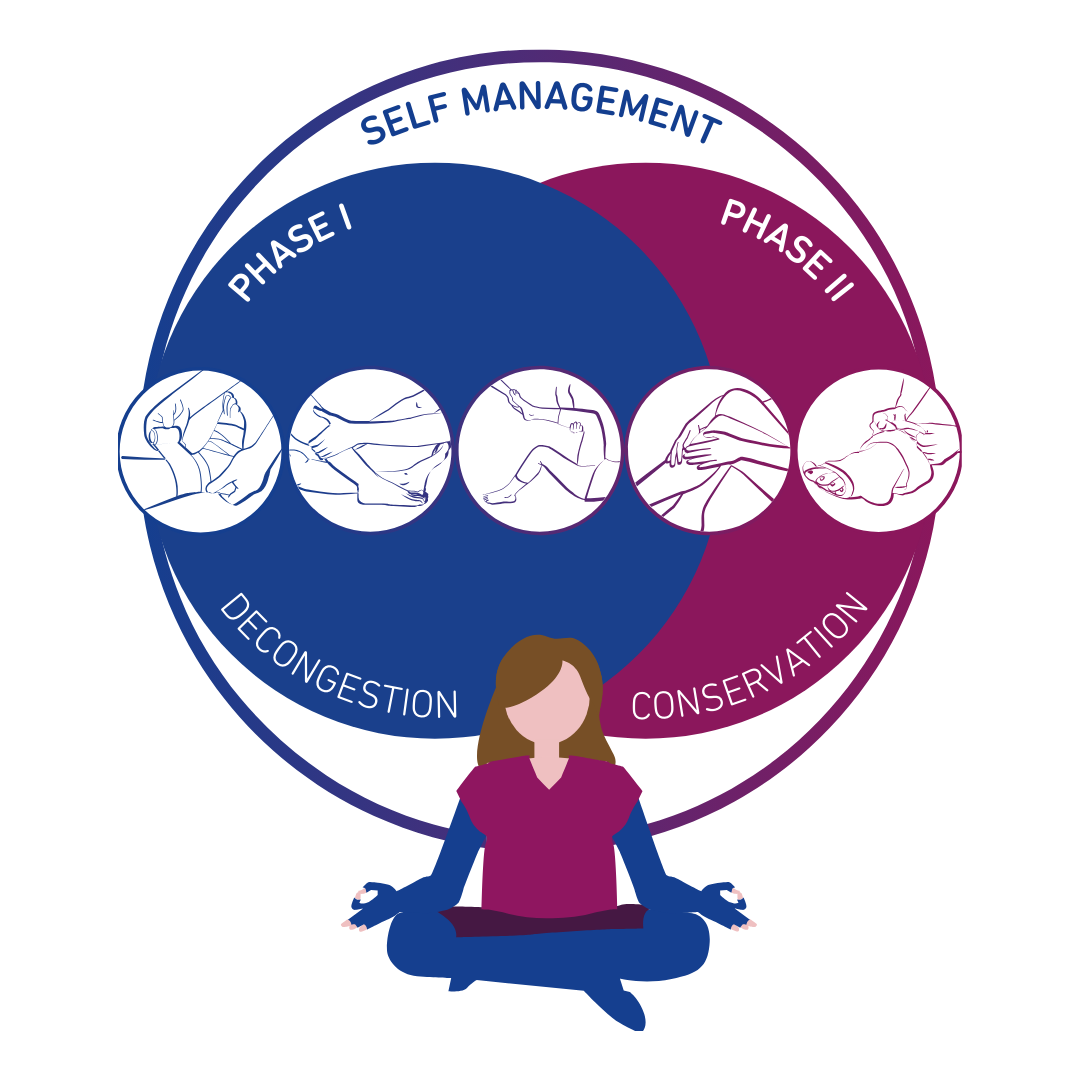
THE FIVE PILLARS OF COMPLEX PHYSICAL DECONGESTION THERAPY (CPT)*
In order to achieve optimal results in lipedema, all subsequent steps must be considered and worked into a therapy routine that is approved by a health professional.
* based on “Self-management of lymphedema” by Lymphselbsthilfe eV
PILLAR 1
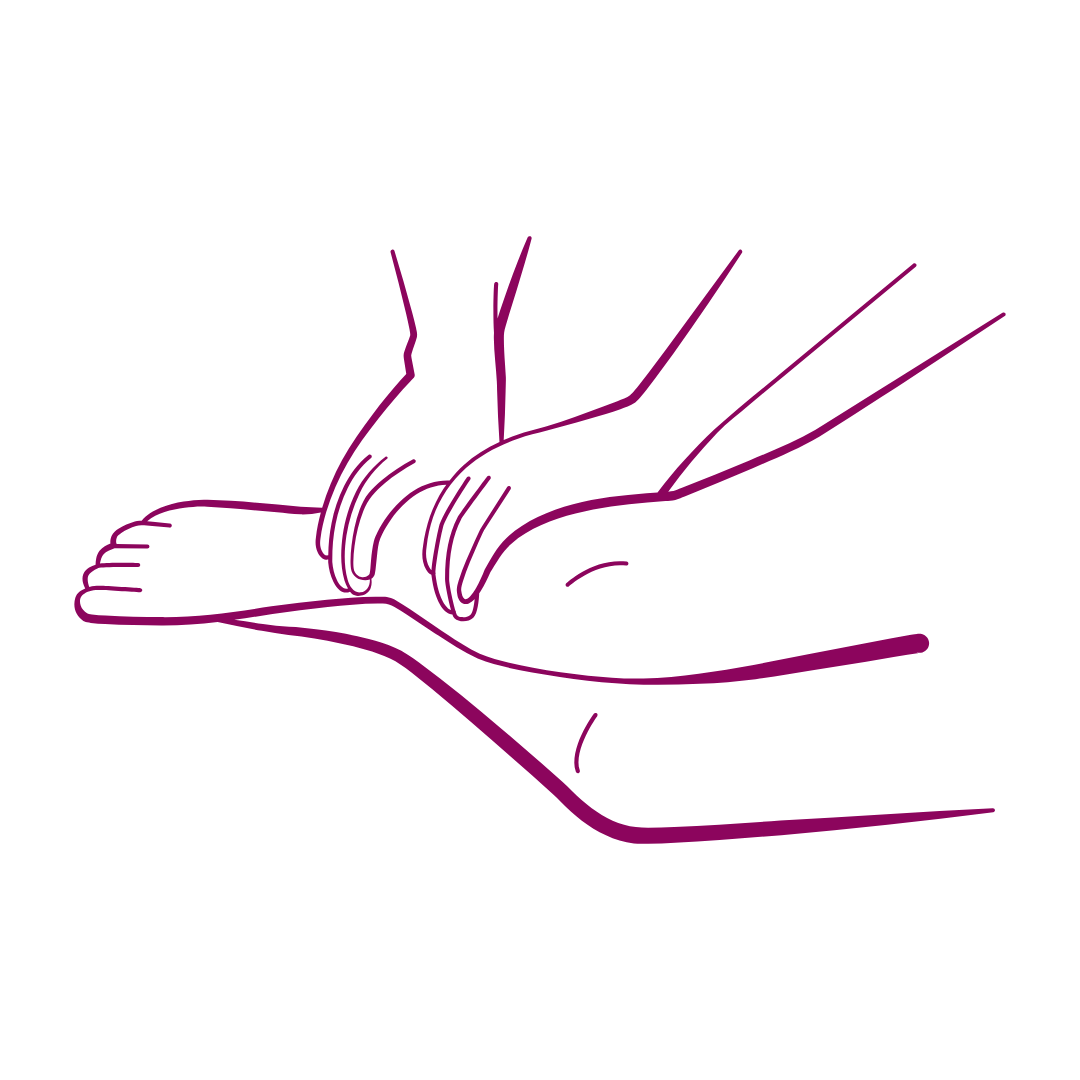
MANUAL LYMPHATIC DRAINAGE
A special lymphatic massage promotes the removal of fluid from the swollen tissue. A physiotherapist carefully massages the lymph into healthy areas of the body from where it can be transported away. Manual lymphatic drainage (MLD) should be carried out multiple a week when possible.
Intermittent pneumatic compression (IPK) can also be helpful as a supplement to the therapy. In it, the affected limbs are surrounded by theraputic sleeves with air chambers that are successively filled up by a device. The pressure from the gradient compression generated relieves the tissue and stimulates the lymph flow.


BÖSL Lympha-mat® 300N
Gradient intermittent compression for specific treatment of lymphatic edema.
The BÖSL Lympha-mat® 300N offers an effective form of intermittent pneumatic compression therapy. Next to manual lymphatic drainage, intermittent pneumatic compression has been firmly integrated as a pillar of current decongestion therapy practises.
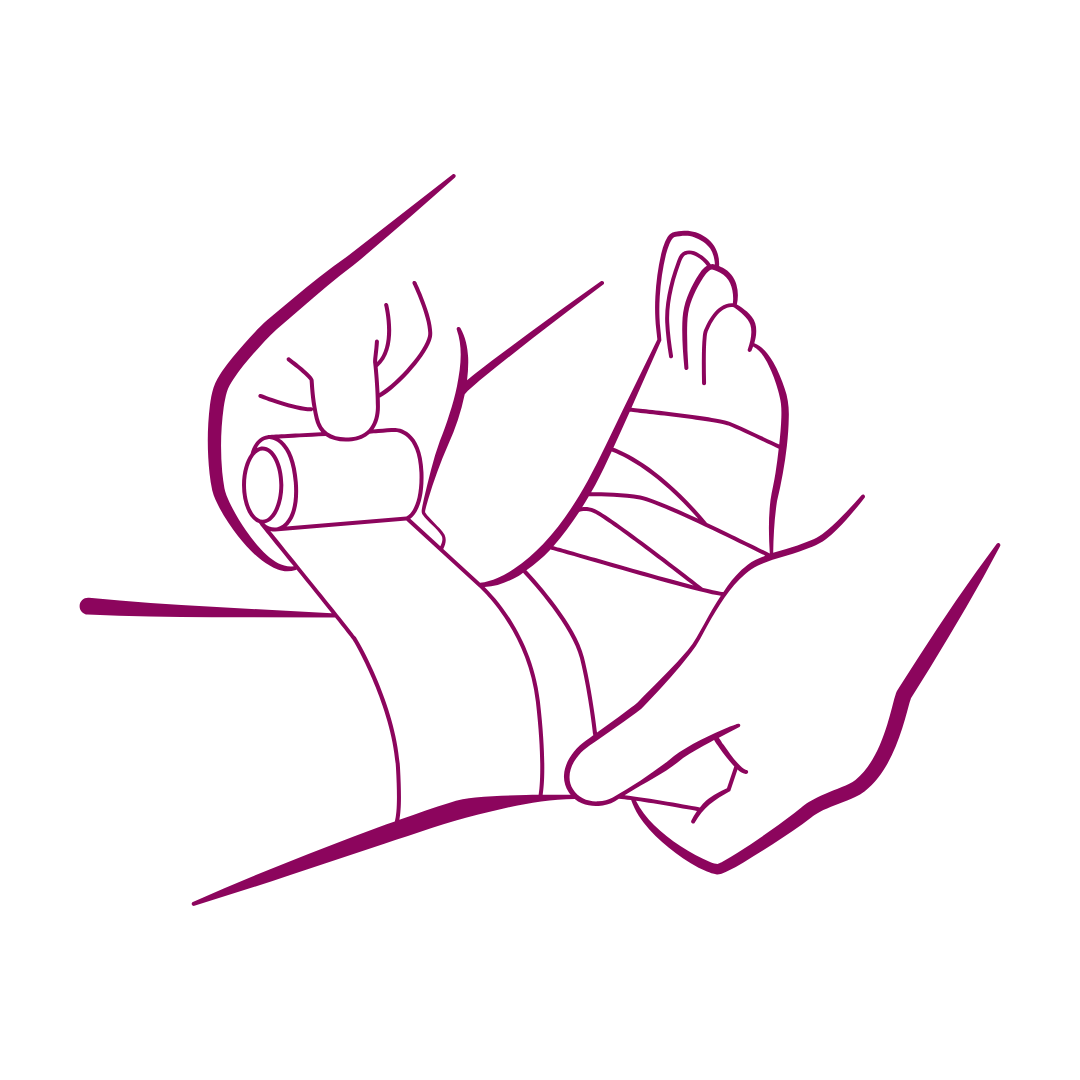
PILLAR 2
COMPRESSION THERAPY
In the decongestion phase, a lymphological compression bandage is applied after each lymphatic drainage. In the maintenance phase, flat-knit medical compression stockings are used. This type of compression therapy for edema prevents fluid from accumulating again, as the external pressure on the skin offers better resistance than the skin alone. In addition, every movement promotes the interaction between muscles, skin and the external pressure. This light massaging effect further improves the removal of lymph. It is important that the individually tailored compression stockings are prescribed by a doctor and professionally fitted by a medical specialist, as the perfect fit is very important. The custom-made compression stockings should be worn daily in order to make the effect noticeable in everyday life and thus to curb the progression of the disease.
THE VENOTRAIN® CURAFLOW SOLUTION
Compression garments for the treatment of edema
Bauerfeind’s flat knit Curaflow compression garments are custom-made and perfectly adapted to the lymphedema or lipedema of the patient’s legs, feet, arms, or hands. VenoTrain® Curaflow compression garments relieve pain and maintain a consistant pressure all with an exceptional wearing comfort!
PILLAR 3
EXERCISE THERAPY
Exercise and movement is an important part of therapy for lipedema and lymphedema. Depending on the type and location of the edema, targeted decongestion exercises and training sessions can improve mobility and reduce swelling. It is important to set realistic goals when creating an exercise plan and discuss with your physician what types of exercise are suitable for you. Yoga, walking, cycling and aqua fitness are some examples of exercises that are gentle on the body and can be a good starting point to include more movement into your daily life.
PILLAR 4
SKIN CARE
The skin of lipedema and lymphedema patients is particularly sensitive. It is prone to dryness, itching, infections, inflammation and impaired wound healing. Therefore, skin care plays a major role in the therapy. It is important to regularly cleanse, dry and then moisturize the skin. We recommend looking for mild products without fragrances and always testing a new product on a small patch of skin before using it on a large area.
PILLAR 5
SELF MANAGEMENT
Because lipedema or lymphedema cannot currently be cured, treatment must be a lifelong process. Patients need a lot of motivation and perseverance to maintain proper management. Extensive knowledge about the conditions and training on the different therapy measures are very important. Psychological support, community social groups and general wellness treatments are also an important part of therapy.
LIVING A CAREFREE LIFE WITH EDEMA!
At Bauerfeind, we are passionate about our products and the amazing people who wear them! When it comes to treating Lymphedema or Lipedema we believe in a holistic approach ensuring that the patient's overall well-being is the most important factor!
Our goal is to create a supportive community to spread knowledge and awareness! We would love to hear about your personal experiences and your favorite feel-good tips!
We look forward to connecting with you!














